Suicide Prevention — What Can We Do?
A Q&A With Thrive’s Clinical Director, Kerstin Trachok, LCPC
Suicide is the tenth leading cause of death in the United States. In 2019, 47,500 Americans lost their lives to suicide, which comes out to about 130 lives lost to suicide per day. Also in 2019, 1.4 million Americans attempted suicide.
Through knowledge, treatment, and support, we believe suicide is entirely preventable. In honor of National Suicide Prevention Awareness Month, Thrive Reno’s Clinical Director, Kerstin Trachok, LCPC, offers clinical insight to help shine a light on suicide prevention.
What signs and symptoms of suicide should individuals be aware of?
Signs and symptoms of suicidal ideation can vary slightly from person to person, but there are certain warning signs of which to be aware.
These signs include:
- Increased depression or low mood, or even sudden changes in mood
- Low energy or sudden change in energy
- Isolation from family and/or friends
- Loss of interest in activities, school, sports, or other things the individual may have previously been interested in
- Change in sleeping patterns: either sleeping more often or struggling to get enough sleep
- Changes in appetite: eating more or less than usual
- Increased feelings of hopelessness
- Saying things such as, “I don’t want to do this anymore.” Or, “I just want to go to sleep and not wake up.”
Another sign that often gets overlooked is a sudden improvement in mood in an individual who has been chronically depressed or suicidal. This does not necessarily indicate that the individual has become less suicidal, but possibly that they have finally decided to commit to a plan of completing suicide.
Additionally, if an individual is getting their finances in order, contacting family members or friends they normally would not reach out to, packing or giving away their belongings, it could signify that they have decided to complete suicide.
Is there a stigma surrounding suicide? How does this stigma hurt suicide prevention efforts?
Unfortunately, there is a societal belief that if we talk about suicide, it will encourage people to complete suicide. This is untrue, and in fact the opposite is true. If an individual is struggling and considering ending their life, not talking about it can lead to even more difficult emotions and isolation. Whereas, if the individual has a safe space to express their feelings, actions can be taken to get them the help they need.
Are there any other challenges involved in suicide prevention?
One major challenge is that people are afraid to ask the direct question of, “Are you thinking about killing yourself?” It is important to be able to ask these hard questions because if the individual who is struggling senses hesitation, they, in turn, may be reluctant to express their feelings and continue struggling internally instead.
What does suicide prevention consist of?
The most important part of suicide prevention is education. SafeTALK and ASIST are free training resources available to everyone that teach what signs to look for and how to address concerns related to suicide.
Changes on a societal level are also important to suicide prevention. The first line of contact for a suicidal individual is often to call 911. Due to the high traffic and severity of calls, the threat of suicide may sadly be deemed as less of an emergency than other calls. In Nevada and many other states, there are local agencies such as the Mobile Crisis Response Team and the Mobile Outreach Safety Team (MOST) that attend to calls relating to suicide and provide in-the-moment mental health care and response. Unfortunately, these programs are not as widely known, so people do not know they exist. As such, more education about the available resources on a local and national level is necessary.
On the clinical level, all mental health providers are required to complete suicide training each year to fulfill continuing education units to renew their licensure, but sometimes clinicians lack resources, support, time, and/or funding to provide the intensive care that individuals struggling with suicide require. Therefore, there are often “hand-offs” of a client from one source to a different source that decreases the efficacy of their treatment. To combat this, more long-term recovery support is needed. While some programs are being developed to improve care, barriers are continually met and they differ from agency to agency.
What can lay people do to prevent loved ones from committing suicide?
People can’t let the fear of talking about suicide keep them from doing so. Additionally, individuals should reach out to seek help from teachers, medical providers, and therapists regarding suicide prevention resources. You do not have to know how to treat suicide nor are you expected to, but being someone who is willing to listen and talk to someone can make all the difference in the world.
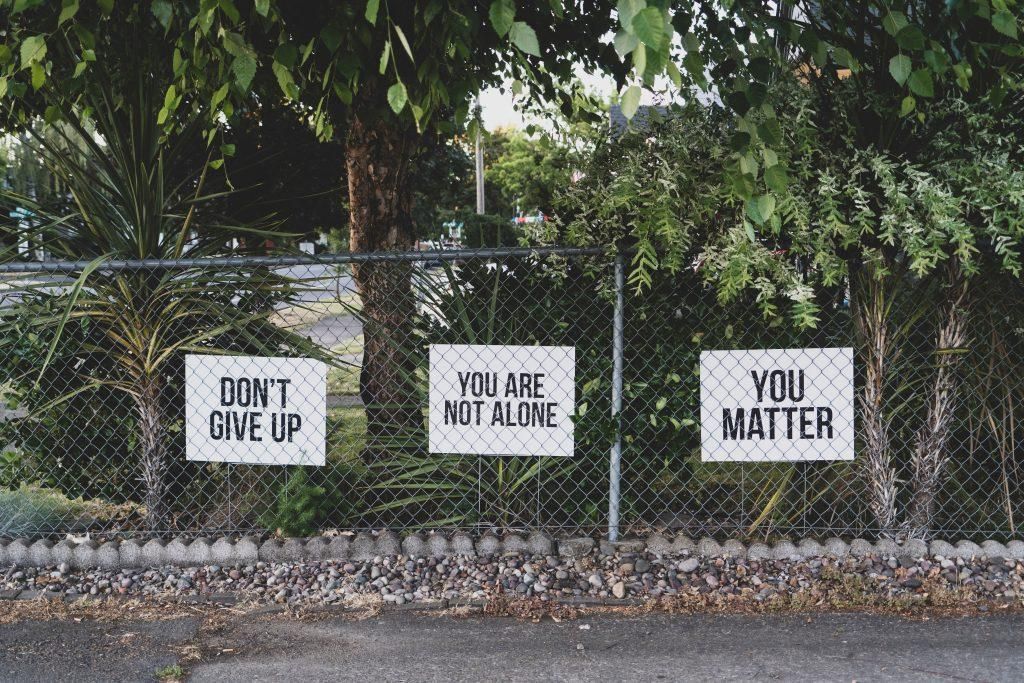
It is also very important to normalize the experience of having suicidal thoughts as most people have experienced them at some point in their lives. Whether there was intention of acting on those thoughts or the thoughts were fleeting during a difficult time, we all have had thoughts of suicide and/or death and dying. Normalizing these kinds of thoughts can reassure people who struggle with suicidal thoughts that they are not “other” or “outside the norm,” but that they are normal, they are not alone, and help is available.
How can mental health providers do more to prevent suicide?
We can remember to not get complacent or comfortable. Even though we may have asked the question of whether the client is struggling with thoughts of suicide a thousand times, not asking the thousand-and-first time could be just enough to miss something important.
Remember to look for the warning signs and increased risk factors for completing suicide. If you are unsure about something, always consult or seek supervision, and do not be afraid of asking the difficult questions.
For individuals with a loved one who may be struggling with suicide, how can they support their loved one’s recovery?
Talk to your loved one, surround them with love, reach out for help if you are unsure, and be sure to take care of yourself as well. When having these types of conversations, it can be difficult to be mindful of your own emotions because you are worried for the person you love. Do your best to stay calm, hear the person out, and respond with empathy.
Reflect your loved one’s emotions by saying things like, “It sounds like you are feeling lonely.” or, “I hear you saying you are experiencing intense feelings of sadness and hurt. I’m so sorry you are going through such a difficult time.” These sentiments can help your loved one realize that you are listening to them and feeling for them.
We often feel that we need to “fix” the person who is struggling and come up with a solution, but that can often feel overwhelming to the individual and cause them to shrink away. So instead, take a deep breath and remember that you do not need to have all the answers, but you can gently encourage your loved one to talk to a professional.
LET’S NURTURE YOUR LIFE TOGETHER
Thrive recognizes the bright spark every individual brings to this world. If you’re struggling to find your spark and are experiencing suicidal thoughts or behaviors, our specialists can help you rediscover hope, joy, and confidence to live your life to the fullest. Please reach out to us for therapeutic support.
If you’re experiencing suicidal thoughts or behaviors, you can also call the National Suicide Prevention Hotline at 1-800-273-TALK (8255).
About the Author
Kerstin Trachok, CPC — Thrive Reno Clinical Director
Kerstin received her master’s degrees in clinical mental health counseling and school counseling from the University of Nevada, Reno. Kerstin has six years of experience in the counseling field working in different settings and a wide array of mental health issues. Kerstin has experience working in schools with children of all ages, clients with psychosis in a hospital setting, adults and teens in private practice, and working at an agency providing counseling to children and families. Kerstin is a fully licensed clinical professional counselor in the state of Nevada and received her certification in Complex Trauma Levels I and II. Kerstin has experience working with children, teens, adults, and families with trauma, anxiety, grief, depression, ADHD, autism spectrum, suicidal ideation, and behavioral issues. Kerstin is passionate about fostering the client’s growth and autonomy while providing a safe and secure space to process emotions. Kerstin uses creative interventions and other tools to allow clients to voice their internal experiences beyond traditional talk therapy. Kerstin’s theoretical approach is Acceptance and Commitment Therapy. She uses mindfulness tools and techniques to help clients be present-moment oriented, and reduce stress so they may move towards psychological flexibility. Kerstin believes all individuals have the right to live a fulfilling and vital life.
The post Suicide Prevention — What Can We Do? first appeared on Thrive Wellness.








