Understanding Obsessive-Compulsive Disorder and Related Disorders
Signs and Symptoms
to look out for
OCD arises when a person becomes trapped in a repetitive pattern of distressing thoughts and subsequent actions to neutralize the distress. These distressing thoughts, known as obsessions, are unwelcome and intrusive, triggering intense emotional discomfort.
Compulsions are behaviors, rituals, or avoidance that individuals adopt in an attempt to alleviate the obsessions and reduce distress levels. Unfortunately, the reduction in distress that compulsions offer an individual is non-existent or temporary at best.
Research indicates that 94% of the general population experiences unwanted or intrusive thoughts and moments of uncontrollable behavior. However, in the context of OCD, these intrusive thoughts occur at a higher frequency, intensity, and duration and elicit intense distress that interferes with everyday functioning.
For a diagnosis of OCD to be determined, the cycle of obsessions, compulsions, and/or avoidance must reach a level of severity where it occupies a substantial amount of time, leads to intense distress, or interferes with everyday functionality, relationships, education, and/or employment.
Obsessions and Compulsions
Obsessions refer to irrational thoughts, fears, or worries that occur frequently and trigger significant anxiety. These obsessions are resistant to logical reasoning and attempts to control them. Some examples of common obsessions include:
- Intense preoccupation with dirt or germs
- Repeated doubts, such as constantly worrying about whether a task has been successfully completed
- Excessive fixation on order or symmetry
- Disturbing thoughts related to violence or causing harm
- Engaging in prolonged periods of touching objects or counting
- Being troubled by thoughts that conflict with personal religious beliefs
- Intrusive horrific images or thoughts
- Intense repetitive fears or worries that are out of proportion to reality
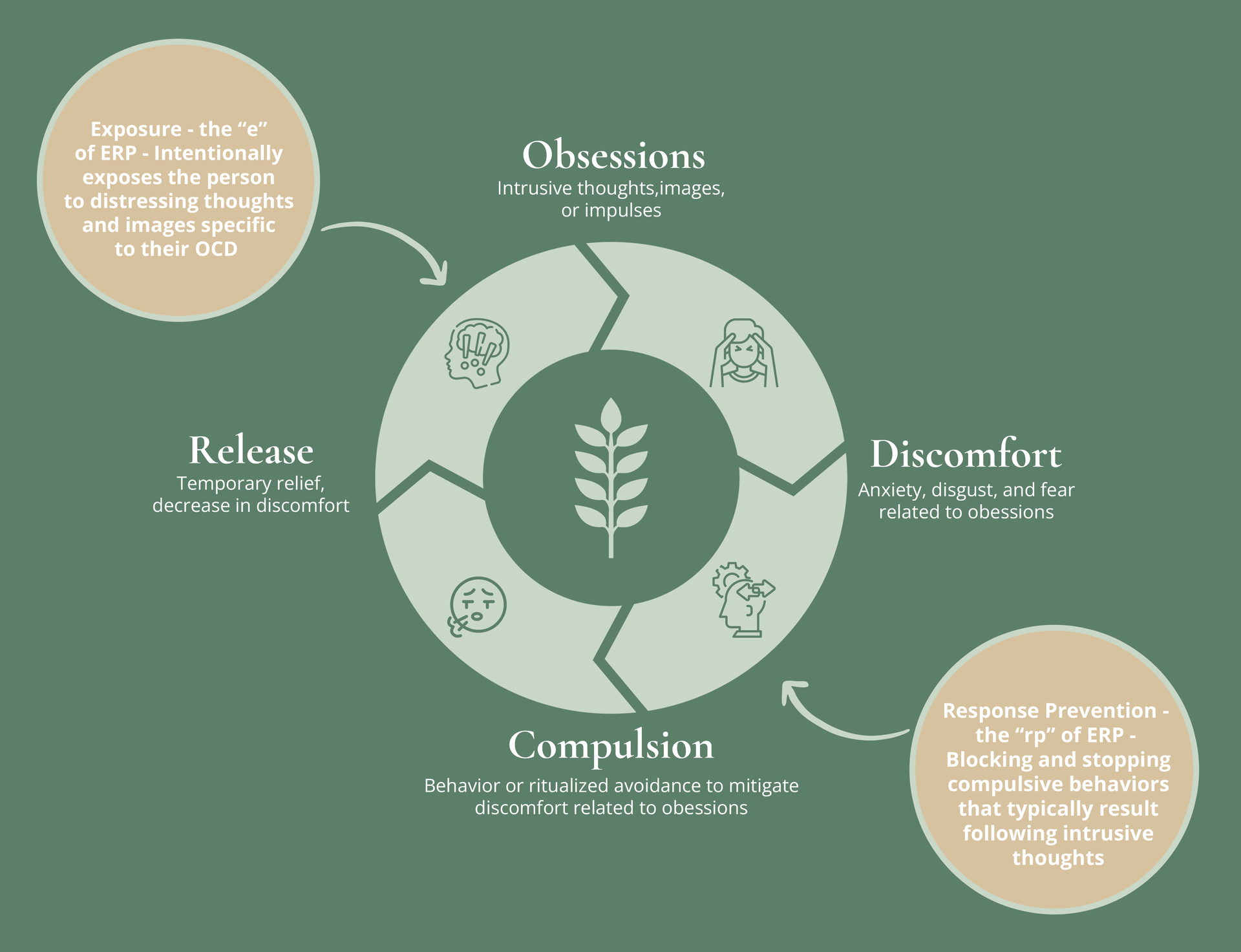
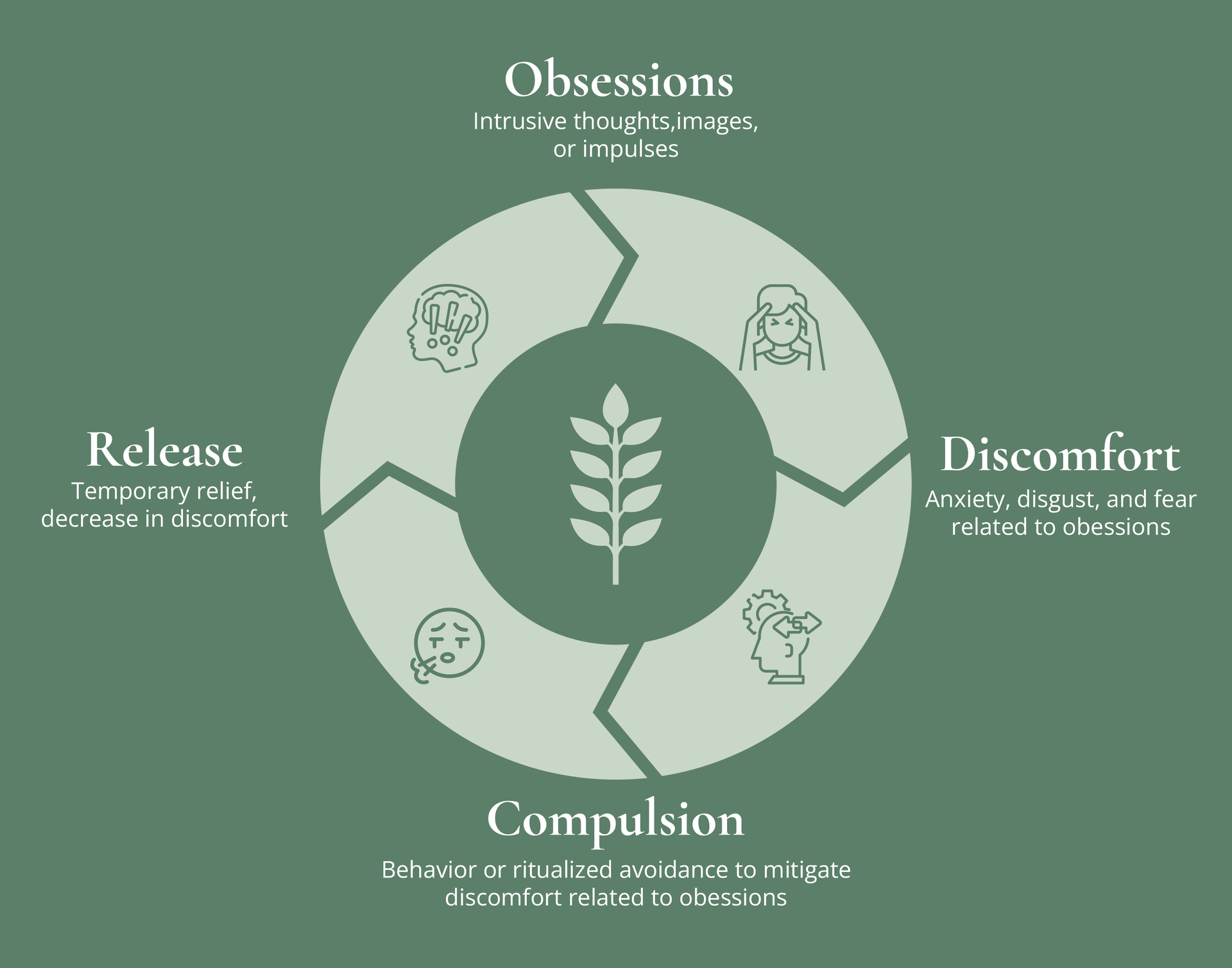
The Cyclical Nature of OCD
The below diagram displays the cycle of OCD. Intrusive and unwanted thoughts (obsessions) are followed by an increase in discomfort. Next, the person engages in behaviors or avoidance (compulsions) in order to reduce the discomfort. This immediately leads to temporary relief-yet reinforces the idea that compulsion is necessary to reduce distress.
Compulsions are behaviors performed with the intention of neutralizing or alleviating the anxiety that arises from obsessions. They serve as coping mechanisms to mitigate the distress caused by the obsessions. Examples include:
- Engaging in excessive showering, bathing, tooth brushing, grooming, or toilet routines
- Counting while performing a task until reaching a specific "good," "right," or "safe" number
- Repeatedly checking to ensure that you have not harmed others or yourself
- Seeking reassurance by constantly telling, asking, or confessing to others
- Repeatedly verifying and rechecking, such as ensuring a door is securely locked
- Adhering strictly to established rules of order, such as dressing in a specific sequence each day
Contrary to finding pleasure in these actions, people with OCD believe that these actions are necessary to avoid negative outcomes or to alleviate anxiety caused by obsessions. Individuals with OCD often possess an awareness regarding the irrational and excessive nature of their obsessions and compulsions on some level. Nevertheless, they experience a sense of powerlessness in controlling their obsessions or suppressing the compulsive behaviors.
Highly Effective, Evidence Based Treatment
When it comes to treating OCD, there are two critical components of treatment: a specific type of Cognitive Behavior Therapy (CBT) called Exposure and Response Prevention (ERP) and medication. Camp Courage utilizes both ERP and, when necessary, medication management to assist clients in recovery. Research consistently demonstrates that when implemented correctly, ERP is effective in over 70% of cases of OCD among children and adolescents. It’s the gold standard psychotherapy for OCD and related disorders with the strongest evidence of treatment success.
It’s crucial to be aware of the most effective and evidence-based treatments for OCD and related disorders to ensure the best treatment outcomes. Not just any type of CBT is effective in the treatment of OCD – in fact – some types of CBT can have the opposite effect. “Cognitive therapy” techniques and “thought-stopping” can even worsen the condition. With an emphasis on reframing or blocking thoughts, cognitive-based interventions often become new mental rituals and intensify struggles with compulsions. Approaches like psychodynamic/psychoanalytic therapy, and interpersonal psychotherapy may also be ineffective or even harmful to individuals with OCD. Working with a treatment team that is trained specifically in ERP is critical for effective OCD treatment.
Where ERP Fits in the cycle of OCD
The Below diagram demonstrates where treatment interupts the OCD cycle. Exposures intentionally introduce unwated thoughts (obsessions). This is followed by an increase in distress. Compulsions are blocked to interrupt the cycle. Discomfort naturally dissipates over time during the exposure, and the brain gradually learns that compulsions are not necessary to reduce distress.
By harnessing the power of ERP, often in combination with medication, we can pave the way to recovery from OCD. By avoiding ineffective methods of OCD treatment and embracing therapies that have proven results, we are able to assist clients living with OCD and related disorders in reaching their best possible recovery outcomes.
Family Intensive Treatment
As a parent, it is your job to keep your child safe, offer comfort, and provide reassurance when they are afraid. It’s easy to assume that providing comfort, reassurance, and soothing irrational fears is the appropriate response to your child’s OCD or anxiety disorder. Parents often assume that continuing in the role of a "comforter" will reduce a child’s distress and ultimately their suffering.
Unfortunately, when it comes to OCD, the opposite is often true. Avoiding situations and scenarios where the child’s OCD and anxiety fears are triggered, offering reassurance, or allowing a child to engage in compulsions to avert conflict only worsens the condition and solidifies these life-interrupting patterns of behavior. In avoiding scenarios that the child fears, offering reassurance, or not interrupting compulsions, you as a parent are engaging in what’s called “accommodation” of the disorder.
In treatment, our clinicians will help you reduce family accommodation that worsens OCD. They will help your child create a “fear hierarchy” together - where feared situations are labeled, rated on a scale of 0-10, and tackled one at a time. With the support of parents, through gradual exposure and blocking compulsions children learn that the feared outcomes of their OCD and anxiety usually do not come true and that feelings of distress they once thought were intolerable become more tolerable.
The Courage to Recover
It takes courage to take the necessary steps towards recovery. Many people need the strong support of their families and loved ones to push them in the right direction. Without this, they often don't pursue recovery. Pursuing the appropriate treatment at the appropriate intensity as soon as possible for OCD is critical for long-term recovery. Based on a large body of research, we know that the sooner a person engages in treatment after the onset of OCD, the more positive the long-term outcome will be. Recovery is possible with specialized treatment for OCD and related disorders, and recovery rates of 70% or greater occur for clients who receive ERP from well-trained clinicians.
At Thrive Wellness, it is our priority to empower our clients and their families with the skills necessary to face OCD and related disorders. Thrive’s ERP-based programs are thoughtfully designed to offer a nurturing and immersive treatment experience for those who are suffering, as well as their families and support systems. Our focus and priority is to provide patients and their support systems with the necessary tools and unwavering support to pave a path towards long-term recovery.
If you or someone you care about is experiencing severe anxiety or OCD symptoms, please don’t hesitate to seek help. The sooner the treatment, the better the outcome!